Mary French and Her Mortal Fight with Colon Cancer

Detection
In the summer of 2019, my mother developed a fever with chronic diarrhea and a sort of burn in her upper abdomen. The symptoms eventually led to dehydration, delirium, and emergency room trips. She was given meds, put on an IV to treat the symptoms, and then sent home. Over the course of 2019, my mother anecdotally described feeling more tired and needing to nap for the first time in her life.
Without data or an in-depth understanding of her reality, I would validate her saying I love naps so that she wouldn’t feel bad about her new need for them (and I really do love naps).
Nearly 9 months later, on March 7, 2020, my mother went for her annual checkup with her primary care doctor, who did all the standard tests and gave mom two thumbs up.
Within a week, she started a fever and diarrhea as COVID escalated. She was told that if she had no trouble breathing to stay home. Eleven days of fever later, a bulge appeared in her abdomen so she went back to the hospital only this time she couldn’t have any visitors. She was admitted to the non-COVID wing, but after her allergies kicked in, she was moved to the COVID area. After nearly two weeks in the hospital which consisted of two COVID tests, two CT scans, and a colonoscopy biopsy, she was diagnosed with late-stage 3c colon cancer. Stage 3c means that cancer had spread to her lymph nodes but not other organs. In mom’s case, that meant 13 lymph nodes were removed. I had trouble getting over the fact that my mother had gone to the hospital with nearly identical symptoms in 2019 without any root cause analysis.
I also struggled with the lack of detection from mom’s primary doctor visit days before her colon cancer fever and weeks before she was diagnosed with late-stage colon cancer.
Mom’s primary care doctor didn’t detect anything unusual.
Jim French
Was The Healthcare System Implemented For Acute Symptoms?
Do we only go annually or when we have acute symptoms? Is the healthcare system prepared to spend money on care based on historical consumer health data? I started researching possible earlier detection methods and found a high correlation between resting heart rate and colon cancer.
I realized that when we go to the doctors, they take a one-time not-at-rest heart rate snapshot at best once a year. A heart rate recorded annually is near useless with no context. How could I have detected a slowly increasing heart rate at rest? I could have bought mom a $100 fitness watch and remotely monitored her activity, sleep, and heart rate.
Related: Monitor Your Resting Heart Rate Using LLIF Software
Simply put, a $100 investment with automated monitoring could likely have helped to detect my mom’s colon cancer at an earlier stage, leading to a better outcome and lower healthcare costs.
Our LLIF goal is to identify deviations from normal over short or long periods and alert our members and their loved ones to reach out to their doctors for earlier detection, hopefully before an abdominal bulge appears.
After my mom’s surgery, she started oral chemo, which resulted in severe diarrhea and delirium again, and more IV hydration treatments that led to swollen feet and sores.
Doctors told us that chemo would only improve her survival rate by 7 percent, but when I questioned them about the time period and whether it was 7% of X% or absolutely 7%, I was told they were not good at math.
I didn’t pursue it because it didn’t matter. My mom could not handle the chemo. Later, I found an NIH study showing a much improved stage IIIc survival rate than doctors had indicated. Doctors and physician assistants must carefully consider their recommendations that balance life and death.
When I questioned [the doctors]… I was told they were not good at math.
Jim French
Medical Surveillance
Doctors told us that my mother would be under surveillance moving forward. That means she will see a doctor every three months with specific checks, including a CEA blood test. I didn’t understand CEA. I wondered if there is a blood test that can measure colon cancer, then why not give it to everyone? I learned that is irrelevant in absolute terms but important if you do a baseline after surgery and look at the changes.
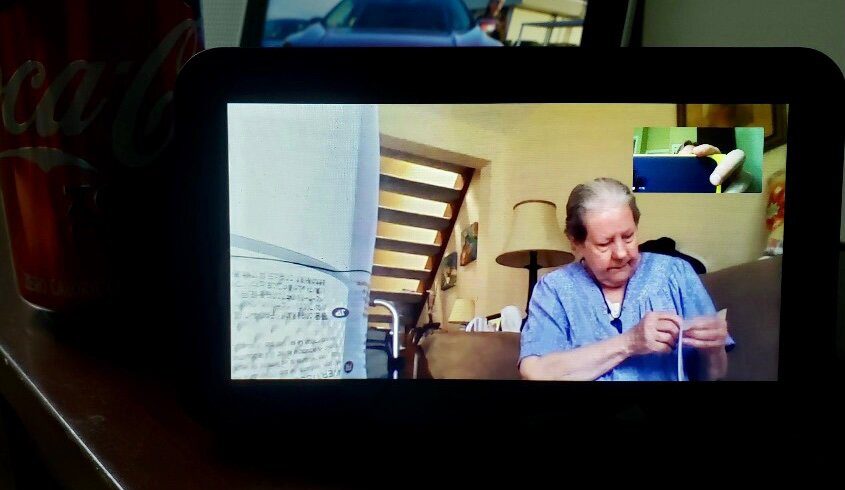
As a result of the battle with cancer, I upgraded mom’s house with Internet (Spectrum has 15 Mbps for $15 senior offer but wasn’t worth it), purchased a cheap $75 Android tablet, got her a $100 Fitbit Charge 3 with a scrunchy band (she can’t work a buckle), and a $100 Amazon Echo Show. Mom is not computer literate, but she is now able to navigate a Roku, manage to charge her Fitbit, answer incoming calls on the Echo, watch photos managed by her kids, and ask the Echo questions.
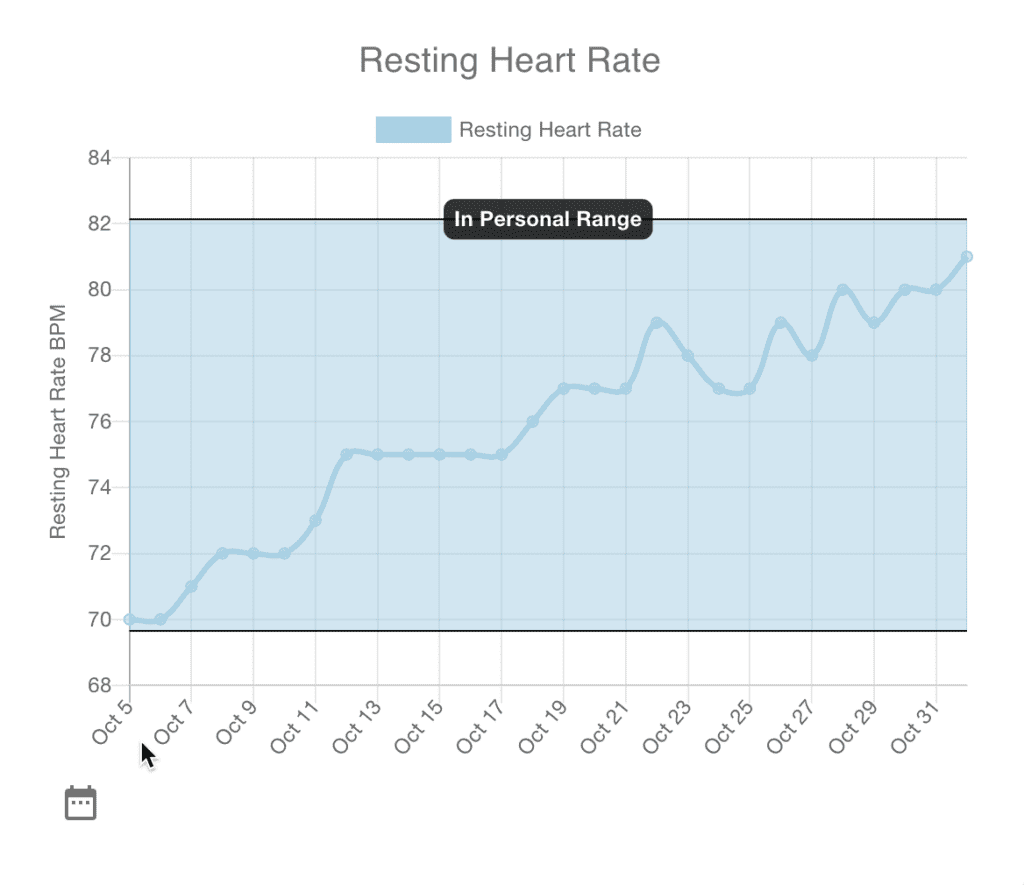
In October 2020, I saw mom’s at-rest heart rate gradually increase by 25% over the course of 4 weeks. I really didn’t know what to do. Should I say something to the doctor? Would the medical community accept a Fitbit heart rate monitor to take action?
Who Knew?
Mom was prescribed two 20mg tablets daily of Famotidine at the start of October 2020. Her heart rate at rest increased by 25% in 4 weeks. After her heartburn symptoms subsided, she was lowered to one pill daily, and her heart dropped back into the low to mid-70s.
Famotidine side-effects include irregular heart rate and rhythm. How often do doctors prescribe medications, and the actual side effects are unknown to both doctor and patient?
At the same time, mom’s sleep scores dropped by 15 percent. Why can’t I monitor my mom and be alerted if her heart rate increases by more than 20% in 4 weeks so I can have an intelligent conversation before calling a doctor? We all know that parents do not share their challenges with their children so as not to be a burden. It’s up to the kids of the elderly to ask the right questions.
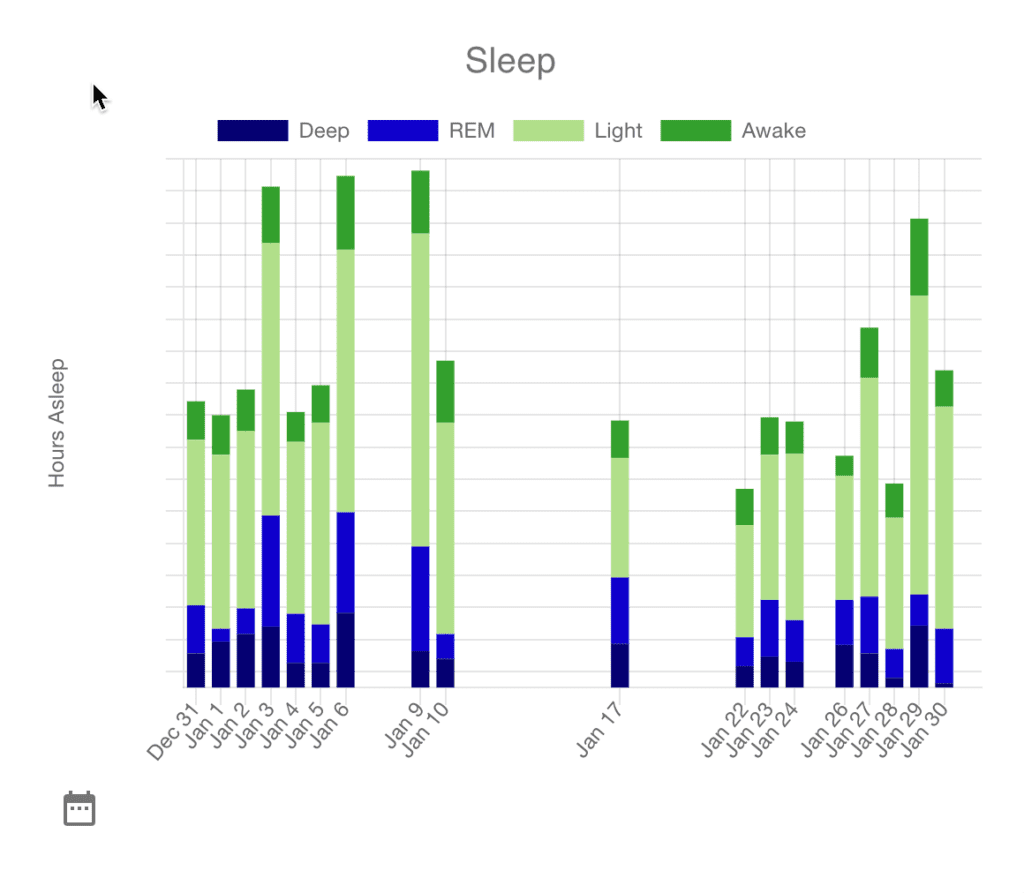
More recently, Mom mentioned she wasn’t sleeping as well, so I looked at her sleep scores and saw that her sleep was so inadequate that it wasn’t even registering as a night’s sleep. I visited her for her 80th birthday on January 24th and again interviewed her. With the data, I learned that she had stopped taking her pain med Tramadol.
Mom went nearly two weeks without registering sleep. Wouldn’t you want to know if your mom barely slept? How would you know even if you asked her? She had said, well, I’ve not been sleeping well, but I didn’t realize how bad it actually was.
Related: Using Best Life to Track Sleep Quality and Sleep Hygiene
Caring For My Mother, Mary French
For eight months during COVID, I finished my basement, anticipating needing to care for Mom. On Mother’s Day, May 9, 2021, the basement was finally done, and I drove to Ohio to get Mom with minimal belongings that would fit in the car since I’d furnished the basement. I quickly got her a car, having left her 2002 Toyota Echo behind. That was not simple since she couldn’t see over the dash of most cars. I got her a scooter to travel from the walk-out basement to her car. I helped her acclimate to the area.
We were hopeful for about a month. In mid-June, we spent many doctor visits focused on Urinary Tract Infections (UTIs). The first diagnosis with a physical examination was a prolapsed uterus, to which mom replied that it was taken out. The doctor said that it must be a prolapsed bladder. Regardless, mom struggled with a pessary for weeks. During these treatments, she started feeling pressure (her term for mild pain), so we weren’t sure if the pessary was causing it.
In mid-July, after ongoing bladder issues, Mom was sent to the hospital for several tests rather than scattering many doctor appointments over weeks. Three days in the hospital is no fun but even less fun during COVID (mom pronounced COVICK). Late on the first day, Mom finally got a new CT scan.
Before leaving Ohio, her medical team had declared her clear of colon cancer due to a CT scan in January 2021, an MRI in February 2021, and a colonoscopy in April 2021. The doctor who read this scan arrived at 7 p.m., just before going home to his family. He had to deliver bad news, but Mom kept changing the subject, so he eventually said, “You’ve got to listen to me,” which angered Mom, so she stopped listening.
So, I heard him explain that she had a tumor the size of a softball or around 4.5”. Mom completely missed it, so I had to explain. I wondered how that could be after she’d been clear from her colonoscopy just three months ago. As we later learned, between the MRI in February and this CT scan, colon cancer grew on her ovary, which was not seen in the colonoscopy.
We later learned the colon cancer grew on one of her ovaries between the time of the MRI in February and the CT scan in July.
Jim French
In August, we had a follow-up with Mom’s oncologist, who put her in hospice care since she was not strong enough for chemo. In late August, her oncologist identified a drug in clinical trials at Duke that may help. The drug was Lumakras, which effectively targeted lung cancer based on a specific marker. Apparently, a few percent of colon patients have the same marker.
It was a long shot, but Mom was tested and found to have that marker. In September, Mom came out of hospice and started on Lumakras. She had a couple of months where her CEA dropped or stayed the same, but it shot back up again. In December, the doctor said we don’t know if Lumakras is working and can’t tell since Mom’s last CT scan was before she started taking the drug. Any tumor growth may have happened prior. We will need to do a CT scan this month and follow up with another one next month to see if her tumor is growing.
The cancer grew substantially that month, so Mom went back into hospice. My son and I had no idea what the coming months would involve as we accepted the responsibility of caring for her at home. In late July, the burden of care was escalating as it took both my son and me to lift her without causing her discomfort. We decided to find a level 3 assisted living care home to take care of her. She was sundowning the day we moved her, and she was convinced that she had been abducted for about a week. After another week, she seemed to be settling in.
However, around August 8, 2022, we noticed the sharp bulge in her abdomen flattened, and she spoke of having vomited blood that day. From that day forward, her pain increased, her heart rate went up linearly, and her communication ability deteriorated. I saw her every other evening and noticed her awareness kept dropping. I planned for August 25, 2022, to spend the entire afternoon with her, hoping to catch her a little more alert.
Related: Track Your Heart Health and Heart Rate
On that day, she was non-responsive, and her breathing was laborious. Immediately, when I sat next to her and held her hand, I told her it was alright and that I was there. She stopped breathing for 30 seconds, stopping my breathing too. I spent the rest of the day there. At 4:00 pm, mom finally did stop breathing after I told her that she lives on within her other children and within me. At 6:01 pm, the nurse pronounced her. She was taken to the funeral home within an hour.
How The Best Life App Helped With Coordinated Care Efforts
In December 2021, LLIF released the first production version of the Best Life app. My son and I were in a situation where two people cared for one person with a very complex medication schedule.
Without getting into the details of all the medications, we had medications that were 4 hours, 8 hours, 24 hours, 36 hours, and as required, with a maximum per week. In addition, we had to track bowel movements, pain, eating, falls, and more. Separately, we used Best Life to track the vitals that were recorded by visiting care professionals.
Eventually, I hired help in the mornings because I couldn’t reliably get a couple of hours to meet with the LLIF team in the morning. So, we had three people caring for mom and visiting hospice workers. My son and I took to logging everything in the Best Life app using events for things we wanted to track, like medications, bowel movements, pain, food, falls, sundowning, and more.
We did not immediately realize the value but quickly learned that it avoided frequent immediate communication required between us. For example, one of us would do something with her and then go to bed, and the other would not have to guess or wake the other up but rather, simply look in the app. With Best Life, we were able to see the latest real-time treatments and take the following appropriate action.
Best Life by the numbers between January and August 2022
- 2698 events were logged
- 318 notes
- 422 doses of Morphine
- 396 doses of Lorazepam
- 214 doses of Famotidine
- 211 doses of Tramadol, which more potent painkillers eventually replaced
- 199 doses of Senokot
- 191 doses of Ondansetron
- 147 doses of stool softener
- 66 doses of Dexamethasone
- 62 doses of Meclizine
- 20 Fentanyl patches
- 60 eggs for breakfast
- 17 fall events
- 11 sundowning events
- 42 buzzes (many not logged)
- Numerous logs of blood pressure (BP), body temperature, and pulse oxygen saturation
The value derived and questions answered thanks to the Best Life tracking app
- How many doses of morphine has mom had in the last week or month? We could use the Event Count graph for the number of doses and now can show the precise amount.
- When was mom’s last fall, or how many times has she fallen this month? We could use Event Count to show the precise count and day of the falls.
- How often has mom been sundowning?
- Is Dexamethasone helping with headaches after her falls?
- Is Meclizine helping to reduce her spinning room experiences?
- Using Best Life, my son and I could associate a drug with reducing headaches from concussions.
- Best Life was invaluable for multiple caregivers regarding as-required drugs that restricted time to the next dose.
- My son and I couldn’t have maintained quality care without constant messages, phone calls, and a shared log.
How Can We Be Better?
Health care
Mom went into the hospital with nearly identical symptoms in the summer of 2019. The medical system simply treated the acute dehydration and did not pursue the root cause. For months before the summer of 2019, through COVID, mom complained of poor sleep and napping.
Unfortunately, I have no record of her at-rest heart rate before 6/2020. I do know that for my own at-rest heart rate, if I eat or drink alcohol after 8 pm, my at-rest heart rate stays 20% higher. The high correlation between resting heart rate and colon cancer exists because if one of your largest organs is struggling, it will show up in your at-rest heart rate when your body is doing absolutely nothing else. I’m more frustrated with our ‘treat the symptom, not the problem’ reactive healthcare approach that led to her late-stage IIIc cancer detection.
I’d already been planning the Live Learn Innovate Foundation LLIF, but this was the tipping point for immediate action. I vowed that if LLIF could help to provide earlier detection for just one other mom, it would be worth my life savings and a decade of my life. Soon, she will be able to log symptoms to her Echo “Alexa, ask life to log diarrhea” along with other symptoms while she’s never learned to operate a mobile phone.
If LLIF can help with early detection for even just one other mother, it will be worth my life savings and more than a decade of time.
Jim French
At LLIF, we hope to productize a similar monitor kit with improved ease of setup and operation and donate kits to those who may not have the few hundred dollars required to purchase one. My mother has been in ongoing colon cancer surveillance every three months. The healthcare system does not know how mom is sleeping, the changes in her at-rest heart rate, her activity level, and truly how often she’s having bowel movements between those visits, but I know that she’s pushing through arthritis pain to get 3,000 to 5,000 steps a day. I love my mom, am impressed by her tenacity, and hope to have her around as long as possible. Over the past nine months, she has seen her CEA go from 3 to 6 to 12, which will mean more tests and possible new actions.

I hope this story has shown that periodic care and monitoring are inadequate. We need to take more responsibility for our care and the care of our loved ones.
At LLIF, we strive to provide the tools needed to achieve proper self-care. We hope to help our members adopt self-care and participate in their family’s self-care team for daily choices, lifestyle, self-manage ailments, minor ailments, and long-term conditions.
Compulsory psychiatric care and major trauma are urgent and require the expertise of our amazing healthcare system, which coincidentally is its strong suit. Let’s fill the gaps elsewhere together.
Ongoing Improvements To Support Personal And Family Care Efforts
LLIF has made or is making improvements to the Best Life app to better support personal and family care use cases.
- Delivered Improvements
- Fitbit sync to replace file uploads
- Events
- Log specific medication amounts
- Log specific drinks and food
- Event durations to log things like sundowning start and end
- Event plans and reminders to make data entry easier and provide reminders for care
- Topic Tags to allow taking care of a loved one in your account
- Planned Improvements
- Shared Topic Tags so my son and I would not have had to log into my mom’s account rather we could have shared a ‘Mary French’ Topic Tag between us and logged mom’s information in a group of two or more.
- We’re adding more detailed pain logging, including nominal and breakthrough pain with location.
- Doctor reports so that a summary of what’s been happening concerning vitals, environment medication, nutrition, symptoms, etc., could be quickly and easily shared with medical personnel.
- Performance reports that will show what caregivers intended to do compared to what they did.
- Quick add for events to make data entry easier
- Alexa voice integration so mom could have logged herself without using a mobile phone which she never mastered. “Alexa, ask Best Life to log tramadol”
- We have a concept called LLIF Extensions (life extensions). Our first is Trend Detection which likely would have shown mom a long-term increasing trend in her at-rest heart rate.
- We will soon support rich text notes.
- We’ll provide periodic high-low average and standard deviation alerts on any variable we collect.
- We’ll support local device alerts if specific data thresholds are exceeded
- We’ll support enhanced diary feed settings to control the display of every data type along with a standard, compact and detailed view.
- We’ll support the ability to correlate a single event against other variables to show the most highly correlated variables.
- Ultimately, we want to open up LLIF Extensions for 3rd parties with the domain expertise to write them. They are architected such that the data and the identity are never shared.
Who we are
The Live Learn Innovate Foundation is a 501(c)3 nonprofit entity that empowers software users to regain control of their personally generated health data, gain intuitive insights about their social data, learn the impact of their environment on health, and build a foundation of data analytics that empowers research, academics, and innovation in economic development.
Use cases for this secure, private data aggregation method appear everywhere, expanding to family care, community growth, agricultural planning, and many more things still unseen. Help us keep going by getting involved today.
3 Responses