In today’s world, where health is at the forefront of our concerns, understanding and participating in breast cancer screening is more crucial than ever. This article, written by breast care specialist Dr. Lauren Mackie, aims to empower and enlighten you with vital information and actionable advice on breast cancer screening.
Whether you’re scheduling your first screening, supporting a loved one, or simply seeking to expand your knowledge, our tips are designed to demystify the process and emphasize its life-saving potential. Join us as we delve into the essentials of breast cancer screening and unlock the power of proactive health management.
Why is breast cancer screening important?
Breast cancer screening is really important, especially for keeping ourselves healthy and safe. It’s like having a trusted friend who keeps an eye out for any trouble, so you can deal with it early. When we talk about breast cancer screening, we’re talking about checking for breast cancer before there are any clear signs or symptoms.
Imagine breast cancer as a weed in a garden. It’s much easier to take care of that weed when it’s small and hasn’t spread. That’s what screening does – it helps find cancer early when it’s smaller and easier to treat. This can make a big difference in getting better and staying healthy.
We understand that not everyone has easy access to doctors or hospitals, and sometimes, it can feel overwhelming to figure out where to start. But even in these situations, knowing about breast cancer screening is helpful. There are often community health programs or clinics that offer screenings for free or at a low cost. It’s like finding a helping hand when you need it.
Remember that taking care of your health is one of the best things you can do for yourself and your family. It’s not just about finding problems; it’s about peace of mind. Knowing that you’re doing something good for your health can be comforting.
Where can I find a place to get breast cancer screening?
If you’re unsure about how to get a breast cancer screening, you can start by talking to a community health worker, a local clinic, or even a trusted friend who might know where to go. It’s okay to ask for help and information. Taking this step is a brave and important way to care for yourself. You’re not alone in this; there are people and places ready to support you.
Dr. Lauren Mackie, DNP, APRN-CNP, is a doctoral-prepared family nurse practitioner with 12 years of experience in general surgery, breast surgery, and preventative care/wellness. She is also a medical freelance writer specializing in breast and other health topics. She can be reached at [email protected] for inquiries.
When Breast Cancer Screening Should Start
The general consensus recommended by the National Comprehensive Cancer Network (NCCN) guidelines and the American Cancer Society is that screening mammography should begin annually at age 40 for average-risk individuals. However, many women need earlier screening.
Females aged 25-39 should have a high-risk assessment to determine when screening should begin, particularly those with the significant risk factors noted below. A breast exam by a provider proficient in clinical breast exams should also be performed by this age.
Females aged 40 and above should have a clinical breast exam and an annual mammogram. Risk assessment should be completed at this time if not performed already.
Risk Assessment Tool
Your provider may use several risk assessment tools to calculate your risk. One of the most common is the Tyrer-Cuzick Model Breast Cancer Risk Evaluation Tool. You can calculate your own risk online as well.
An estimated lifetime risk of <15% is low risk, 15-19% is intermediate risk, and ≥20% is considered high risk.
If you are in the high-risk category, screening mammography and breast MRIs should begin ten years before the youngest family member was diagnosed with breast cancer. The earliest ages you can have these tests are mammography at age 30 and breast MRI at age 25. Your provider will discuss other risk-reducing measures if you are ≥20%, including the possible need for genetic testing, risk-reducing measures, and referral to see a breast specialist.
Risk Factors
Family history of breast cancer is important, but also plays a smaller part than you might think in hereditary breast cancer. Only about 5-10% of breast cancer is caused by a genetic pathogenic mutation.
Other risk factors include:
- Menstruation before age 11
- Menopause after age 55
- First childbirth over age 30
- Prior abnormal breast biopsy (pathology report reading atypia or lobular carcinoma in situ)
- Nulliparity (no biological children)
- Chest radiation therapy between ages 10 and 30
- Ashkenazi Jewish heritage
One in 40 Ashkenazi Jewish women has a BRCA gene mutation. Mutations in BRCA genes raise a person’s risk for getting breast cancer at a young age, and also for getting ovarian and other cancers. That is why Ashkenazi Jewish women are at higher risk for breast cancer at a young age.
CDC.gov
Do men get breast cancer?
Breast cancer in men is rare, and accounts for only about 1% of breast cancer in the United States. Men can also be at risk for breast cancer, particularly if they are a carrier of a genetic mutation that increases their risk. Anyone with a strong family history of breast, ovarian, pancreatic, or prostate cancer particularly in first degree relatives at young ages, should consider genetic testing. Multiple family members on the same side with these cancers raises the risk of a genetic mutation.
Should men receive breast cancer screening?
Yes! If a man has any of the below potential signs of breast cancer, a mammogram should be obtained as well.
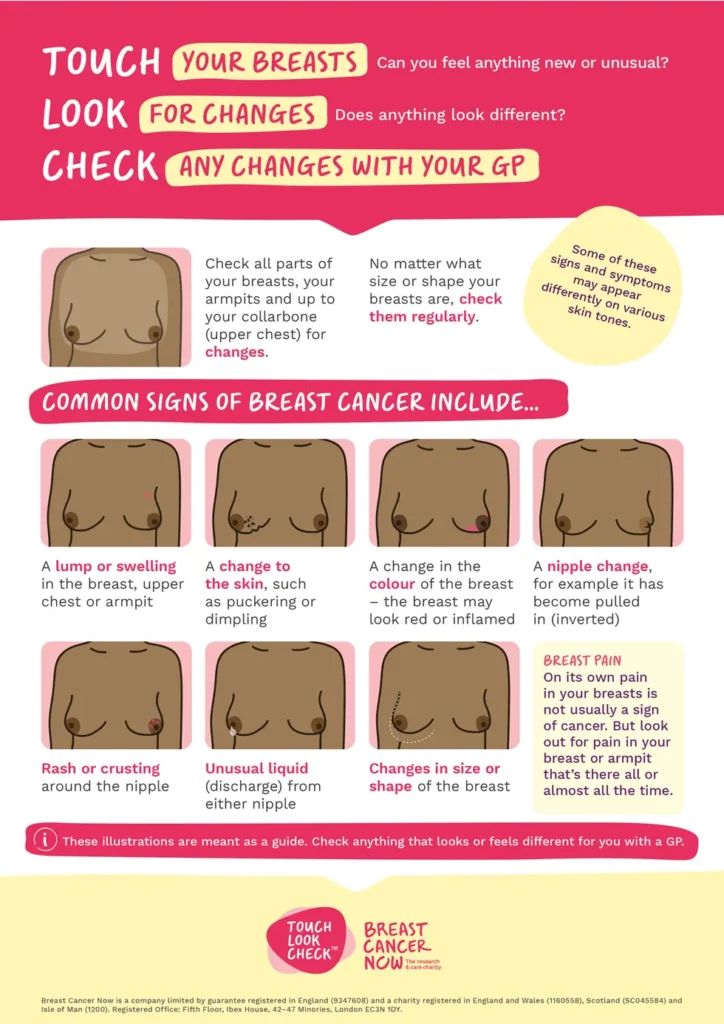
Signs of Breast Cancer
While the below may not always indicate cancer, each should have the proper diagnostic workup. Tell your provider right away if you notice any of these abnormal breast changes:
- Palpable mass/lump
- New nipple inversion/retraction
- Skin dimpling (orange peel appearance)
- Nipple discharge (spontaneous and clear or bloody)
- Nipple crusting
- Redness
- Swollen breast/change in size or shape
- Skin texture change/increased thickness
Related: How does a symptom diary improve medical care?
How Is Breast Cancer Screening Done?
Next Steps
First, if you notice any of the signs of breast cancer mentioned above, don’t panic! Many of the listed conditions are related to benign breast findings. However, every abnormal symptom should have a workup for certainty. Notifying your healthcare provider or gynecologist is best. They can order diagnostic imaging and make referrals to a specialist if necessary.
Breast Cancer Screening: Imaging
If you are over 30, a diagnostic bilateral mammogram and limited ultrasound of the affected breast(s) should be ordered. The two exams are used together, as often times an irregularity is seen best by one modality. In certain circumstances, depending on the radiologist’s recommendation, a breast MRI may be warranted.
If you are under 30, only an ultrasound is performed. Mammography is typically contraindicated in this age group unless otherwise recommended by the radiologist.
A breast biopsy is necessary when the area in question is suspicious of malignancy.
Breast Cancer Screening: Common Breast Findings on Imaging
- Cyst (simple, complicated, or complex)
- Fibroadenoma
- Breast calcifications
- Intramammary lymph node
- Asymmetry (focal, developing, or global)
- Architectural distortion
- Fat necrosis
- Irregular indeterminate mass
- Non-mass like enhancement
- Dense tissue
These findings may be reported on your mammogram, ultrasound, or breast MRI. There is a risk category called BI-RADS that determines the next steps.
BI-RADS Scale on Imaging
The Breast Imaging Reporting and Data System (referred to as BI-RADS) is a classification of how benign or suspicious image findings appear. Determined by the radiologist, it is a guide in ordering the next necessary steps or procedures.
This information can be found at the bottom of your imaging report on mammogram, ultrasound, or breast MRI. It is broken up into the following categories:
- BI-RADS 0: More imaging is needed before a recommendation can be made.
- BI-RADS 1: Negative, no abnormality found (0% cancer risk).
- BI-RADS 2: Benign, the finding is considered benign (0% cancer risk).
- BI-RADS 3: Probably benign, the finding is most likely noncancerous (<2% chance of cancer risk)
- BI-RADS 4A: Low suspicion of malignancy (2-10% cancer risk)
4B: Moderate suspicion of malignancy (10-50% cancer risk)
4C: High suspicion for malignancy (95% or higher cancer risk)
- BI-RADS 5: Highly suggestive of malignancy (95% or higher cancer risk)
- BI-RADS 6: Biopsy-proven malignancy
BI-RADS 3 is very common; the recommendation is to repeat the imaging in 6 months to assess for any change. If the lesion is unchanged or stable, the 6-month follow-ups continue until there has been two years of stability. At this point, the lesion is considered benign.
Be Your Own Best Advocate
Common advice you should not listen to:
- You are too young for breast cancer.
- You don’t have a family history, so I wouldn’t worry about it.
- It’s probably a clogged milk duct.
- This can wait until your mammogram.
- It feels normal to me, imaging is not necessary.
The truth of the matter is that no one can predict what is going on unless you seek the proper examination and workup. Your provider may not want to worry or alarm you. However, seeking a second opinion not only provides peace of mind, it could also save your life.
You can easily track your health, symptoms, signs, and treatments using a health tracking tool like the Best Life app.
Sources
Breast Cancer Screening and Diagnosis
Frequently Asked Questions About the American Cancer Society’s Breast Cancer Screening Guideline
Genetic Risk Factors for Breast Cancer
International Breast Cancer Intervention Study: Risk Assessment Tool
Mammograms for men: What to expect
Six Months Seems Optimal for Follow-Up Imaging of ‘Probably Benign’ Breast Lesions